Home » Obesity Medicine
Obesity medicine combines science-based medicine with attention on the pathophysiology of excess fat accumulation with individualized treatment. Obesity medicine acknowledges that obesity is a complex multifactorial medical condition which carries other health risks and deserves treatment other than telling the patient to just “eat better and exercise”. Yes, nutrition and physical activities are often two pillars of the treatment plan but so are behavioral interventions and medications when indicated as well. Obesity medicine seeks to take away the stigma associated with excess energy accumulation. Obesity is a biological process and not a personal choice or a lack of character or deficit of willpower. In 1948 the WHO/ World Health Organization recognized obesity as a medical condition. It was not until 2013 that the American Medical Association acknowledged Obesity as a medical entity. There are probably many forces that are leading to an increase in body weight at the population level. The cause of obesity in the individual likely varies and does have some epigenetic / genetic predisposition but it is clear current food environment, lifestyle and other biological factors are at play as well. Changes to the gut microbiome, hormone balance and the immune system all likely play a role in the development of obesity.

Over 72 million US adults meet the criteria for the diagnosis of obesity. The estimated cost per year of this epidemic is an additional $ 147 Billion dollars in medical care. This is likely a gross underestimate and seems to be increasing.
The below map from the CDC website estimates the self-reported incidence of obesity by state as a percentage of the population. This is a dramatic increase over the last 20-30 years.
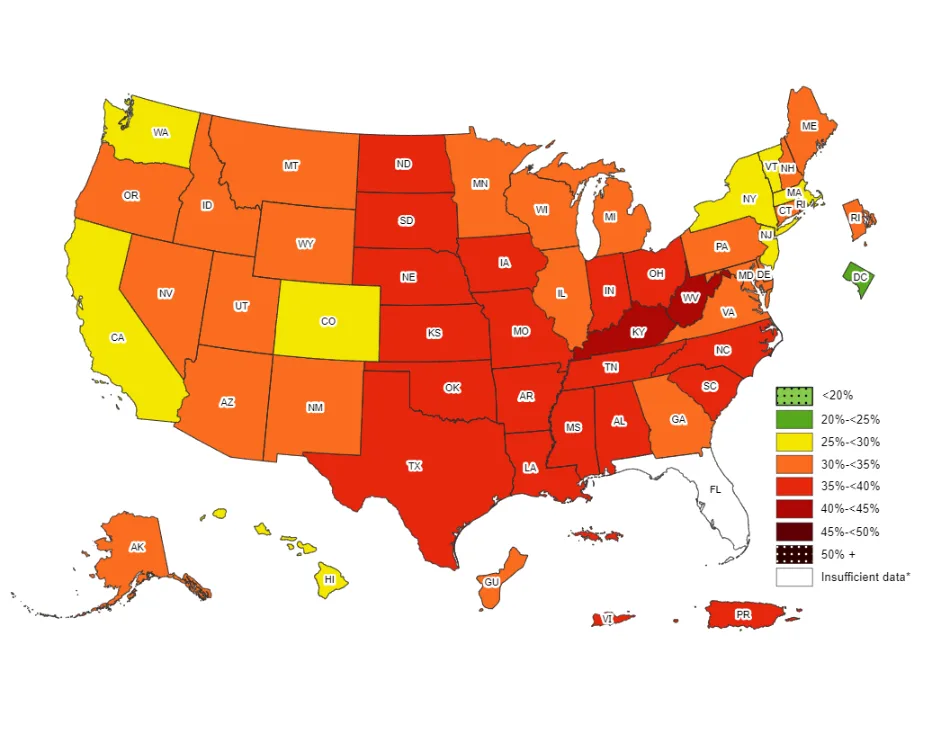
https://www.cdc.gov/obesity/data/prevalence-maps.html#overall
An argument can be made to address and treat obesity first as it impacts risk for over 200 other conditions and diseases including heart disease, diabetes, and even 13 different types of cancer. Obesity is associated with a shortened lifespan of about 7-8 years. We know that the pathophysiology that is occurring affects all cells in the body. The immune system, hormones, cardiovascular system, musculoskeletal system, gastrointestinal system, and neurological systems are all impacted by this one medical condition, so it makes sense to address it first. Treat obesity and often you improve the health of all those systems!
The four components of obesity medicine treatment are the following:
1. Nutrition- The quality and quantity of energy intake matters when it comes to obesity treatment.
2. Physical Activity- Energy expenditure also matters as does percentage of body fat and muscle.
3. Behavioral- So much of what we do day in and day out that make up our lifestyle are points of intervention in the treatment.
4. Medication- As a medical condition, sometimes changes to nutrition, activity and behavior are not enough and medications can be helpful to gain traction in treating this condition.
It is important to address all four pillars in an obesity treatment program as the sum of all these interventions is greater than each individually. As a relapsing type of condition- for example it is not uncommon for a person to gain and lose the same 20 lbs. over and over, we need all these factors to support long lasting treatment success. When we lose weight, the fat cells shrink but it does not go away. Our body has mechanisms for survival of drought and famine that biologically increase energy accumulation once those fat cells shrink. This is why sustainable weight loss is hard * but not impossible when we combine the four pillars of treatment.
Here at Sparkle Health, Dr. Elisa Mercuro, DO and our team have developed The Functionally Fit Program. This program takes the 4 pillars of Obesity Medicine and wraps them in a fail-safe, full support system. On top of addressing and each of the four – Nutrition, Physical Activity, Behavioral, and Medication – we first dive into all possible root causes of a person’s additional weight. Partnering with each unique individual to create a clear, comprehensive medical and emotional life history timeline. Scouring through each detail to detect obstacles that are getting in the way of weight loss. Once discovered, all specific past events, health history, stressors, lifestyle changes, and medical conditions are taken into consideration when creating a person’s customized health plan. This assures a thorough understanding of each person, their needs, and the obstacle they need support around to overcome. Applying the four pillars to these underlying issues can result in much improved overall health, including weight loss.
Another added benefit of our Functionally Fit Program is group classes and the accountability created when having a great support system. Doctor supervision is one of the most important aspects of our program and sets it apart from most others.
Along with all this unique support, our program includes a weight, loss, toolbox including guidebook, app for tracking, menu ideas and recipes, supplements, supporting metabolism, classes, that target weight dysregulation, pharmaceutical support if needed, continuous glucose monitoring, doctor, supervised troubleshooting and medication management, a holistic approach, and a personalized experience that includes ongoing maintenance and support.
Functionally Fit takes a whole-person approach to weight loss. Many of us have struggled to lose weight and have felt frustrated with the many obstacles that can get in the way of weight loss. Whether its stress, lifestyle, diet, or other medical conditions, Functionally Fit treats the underlying issues resulting in better overall health, including weight loss!